By Dr. Alan Palmer
I am doing this article because of the irrational amount of fear I am personally seeing being expressed by relatively healthy people in and near my age group. I am also seeing extreme paranoia around the risks for young people and children. For very elderly individuals and those with serious chronic diseases extra concern and precautions are warranted, but for most the exaggerated level of fear is unwarranted. For much younger people, especially those without the co-morbidities of obesity, hypertension, diabetes or respiratory disease, the risks of serious or fatal COVID-19 illness is infinitesimally less. Sure, there is the rare outlier. You know, the one that people tell you about when they say something like “I heard about a 20-year-old on the news that died from COVID-19”. The reporting on those cases is purely sensationalism because they are so rare. In fact, one thing I am highly recommending is to avoid watching the mainstream media news outlets. They perceive their job as finding the worst story of the worst, somewhere, anywhere and characterize it as a preview of coming attractions near you. In a strange sort of sick way, fear and sensationalism sells. And as long as people continue buying, they will keep selling. I prefer to look at the facts derived from actual data and put those facts into perspective.
What is the actual risk? Let’s look at the raw data, the true facts. I want to be very clear here. When I discuss deaths in this article, I am in no way minimizing loss of life. Each life is precious. Each life is valuable. I am merely citing facts and statistics. Aside from COVID-19, the sad but true fact is that nearly 3 million people die in the U.S. annually from all causes and the oldest among us represent the vast majority of those deaths.
Are the death figures accurate?
The death toll from COVID-19 is mounting and is a major driver of fear, but there is more to that story than meets the eye. Many people are unaware that the criteria for filling out death certificates was changed just for COVID-19. This was done in March by the National Center for Health Statistics (NCHS), deviating from the way deaths from all causes, including respiratory infections have been reported for the previous 17 years.
Here is some of the language from the directive that went out from the National Vital Statistics System COVID-19 Alert No. 2, March 24, 2020.
- “The underlying cause depends upon what and where conditions are reported on the death certificate. However, the rules for coding and selection of the underlying cause of death are expected to result in COVID-19 being the underlying cause more often than not.”
- “If the death certificate reports terms such as “probable COVID-19” or “likely COVID-19,” these terms would be assigned the new ICD code (indicating COVID). It Is not likely that NCHS will follow up on these cases.” (My comment: Now why would they feel the need to say that? It infers, don’t worry if it isn’t correct because no one is going to be checking your work)
- “COVID-19 should be reported on the death certificate for all decedents where the disease caused or is assumed to have caused or contributed to death.”
- Again, this is a clear departure from the way cause of death has been reported previously, when actual cause of death was verified and confirmed.
That document can be accessed here:
Minnesota State Senator and medical doctor Scott Jensen M.D. was all over the alt media and Fox News sharing about this very disturbing issue. Dr. Jensen has even taught medical coding, so he has expertise in this area. Dr. Jensen said in his 40 years of practice, he had never been “coached” or “massaged” to fill out death forms in a way that way completely uncharacteristic of all previous norms. He was interviewed by well-known motivational/inspirational guru Tony Robbins about this situation also. You can see that interview here (if YouTube hasn’t removed it: https://www.youtube.com/watch?v=1CZzdSzUZLE
As a result, suffice to say that the reported number of deaths attributable to COVID-19 are drastically inflated. Why would they do that? Why would they manipulate the numbers? Let’s set that aside and get back to the actual risk.
As with anything in life, there is risk we assume. Every time we get into an automobile, we assume a risk of being seriously injured or killed. Every time we cross the street, we assume a risk. I will compare the risk of dying from COVID-19 to these and other risks we take daily later in this article.
What I intend to show, is that you not only have to consider the risk based on percentage of all deaths assigned to COVID-19, BUT and importantly you then need to take into consideration age, comorbidities and ethnicity. Each of those things play a major role in severity of COVID-19. As an example, if you are 70 years old, age is a factor. But if you are healthy and without comorbidities, COVID-19 is less dangerous for you than the overall risk for your total age group. For those that have been living a healthy lifestyle, it truly will pay dividends in this scenario.
Worse of all, ongoing fear suppresses the immune system making a fearful person at higher risk of contracting COVID-19, because their immune system can’t respond rapidly and as effectively to exposure. But even worse, they are setting themselves up for a more severe case if the virus can gain a foothold in their body because their immune system is dysregulated and suppressed. Yet, everyday I see people so fearful, that they are wearing face masks driving in their cars by themselves, walking, running or riding bicycles in the open fresh outdoor air, far from other people. The level of irrational fear is epidemic. That is one of the main reasons I wrote this article. I hope to help those people that have an open and logical mind, to understand that they can return to a comfortable level of peace and rational-based calculated risk, similar to the way they did for the seasonal flu in years past, observing all of the common sense precautions like hand washing, not touching your eyes, nose or mouth with unwashed hands, etc.
Advanced age is a risk factor
What is the risk of dying from COVID-19 in a given number of people of an age range, WITHOUT taking into consideration any comorbidities? The CDC data below dated August 08, 2020, is the latest reported on the Infection Fatality Rate (IFR) for COVID-19.
For the older crowd there is increased risk. But how much more risk? And, how does that relate to the risk from the seasonal flu? The annual flu was a concern every year, but we never locked the nations of the world down over it. I am also going to show your risk based on the level and number of comorbidities shown to make COVID-19 more serious and potentially fatal.
Let’s first take a look from 30,000 feet at the relative risk for people under a certain age according to CDC statistics reported June 7th, 2020:
- People under 45 years of age account for only 2.5% of ALL COVID-19 deaths!
- People under 55 only account for 7.3% of all COVID-19 deaths.
- People under 65 account for 19.27% of all COVID-19 deaths.
- People 65 and over account for 80.73% of all COVID-19 deaths. (65-74 = 20.77%, 75-84 = 26.64%, 85+ = 33.32%)
Risk for various age groups
Next let’s look at death rates by age groups and the numbers I prefer to look at, the survivability numbers. That means, what is my chance of surviving if a given number of people in my age group are infected with COVID-19? I am hoping that this will help to put it in another context for you and allow you to compare survival rates with fatality rates for your age category.
Age SURVIVAL rates Death rates What does that mean in practical terms?
0-19: 99.997% 0.003% If 34,000 people were infected, 1 would die
20-49: 99.98% 0.02% If 5,000 people were infected, 1 would die
50-69: 99.5% 0.5% If 200 people were infected, 1 would die
70+: 94.6% 5.4% If 20 people were infected, 1 would die
https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html
Let this sink in a minute
A CDC page titled, COVID-19 Hospitalization and Death by Age, compares risk of different age groups. The rate of death from COVID-19 in those 85 and older is 630 times (63,000 percent) greater than 18-29-year-olds. And, it is approximately 5,670 times (567,000 percent) higher than children aged 0-4 and 10,080 times (1,008,000 percent) higher than youth aged 5-17!
If you are over the age of 70 and certainly if older than 85, there is cause for genuine concern. But there is also cause for genuine concern in those age groups with the seasonal flu or pneumonia. And, consider that nationwide 40% of deaths have occurred in nursing and long-term care facilities. In some states those deaths are higher, ranging as high as 82% of deaths as is the case in New Hampshire. https://www.kff.org/coronavirus-covid-19/issue-brief/state-data-and-policy-actions-to-address-coronavirus/#long-term-care-cases-deaths
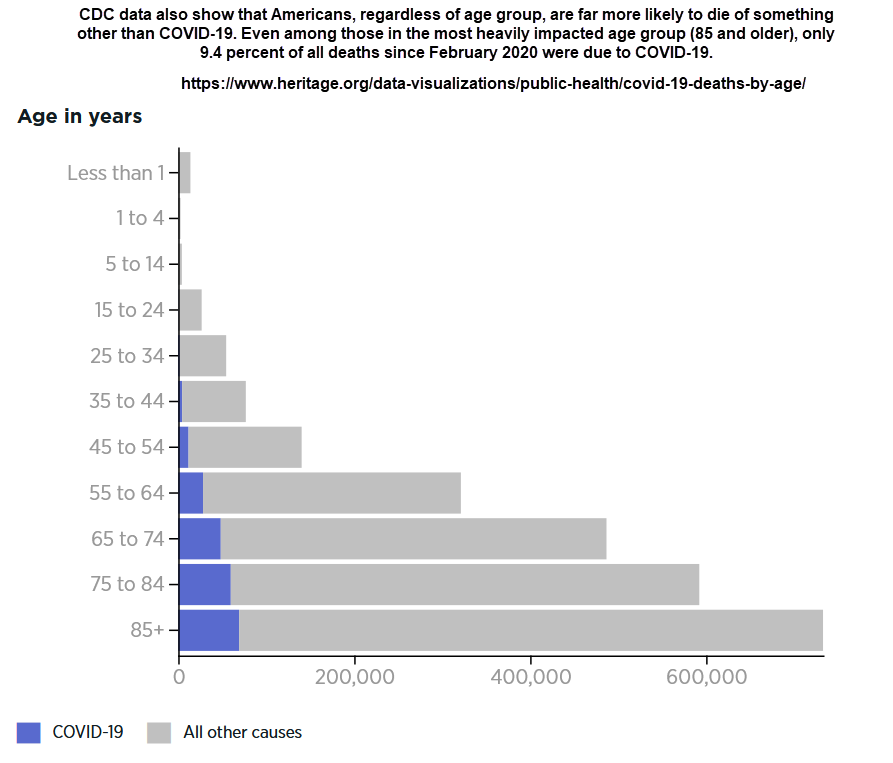
One thing to consider when speaking of the very elderly dying from COVID-19, is that the average life expectancy in the U.S. is 79 years and people are much more likely to die of something else rather than COVID-19. The following graphic displays that fact and also shows the proportion of the COVID-19 deaths in the U.S. based on age ranges.
Lockdowns, masks and extended isolation is not the answer
One of the rationales for locking down society, wearing masks, closing schools (even those for young children) is, “we want to protect grandma or grandpa”. The stark reality is that all of the measures we have taken have not made the virus go away. It is just prolonging the whole process, the misery so to speak. And the most recent studies suggest that the lockdowns don’t even reduce mortality and the facemask mandates do not slow the spread of infections, so what is the point? (see some recent references at the end of the article about that). At best, they may only delay the time it takes to spread. Yet, the lockdowns are having devastating effects emotionally, physically, economically, relationally and causing untold deaths (even thousands of young and middle-aged people from a variety of sources related to lockdowns).
We absolutely need to protect those that are elderly and those with serious metabolic disease by quarantining them. To get beyond that, around 30-40% of the population will need to contract the virus, recover and have long-term immunity (which many studies say they will). This should comprise mainly of the healthy under 60 age group. In addition, we can add to that number another 30-40% of the population that already has a good level of T-cell immunity from previous coronavirus (common cold) infections which will provide a robust amount of protection from SARS-CO-V-2.
Of course, some will argue that a vaccine can help us reach that population or herd immunity levels. This is a very complex discussion and far beyond the scope of this article. But I will say that with a rushed to market (10 months vs. 4-6 years), incompletely tested (especially for long-term side effects like autoimmune disease), never tested in humans (Messenger RNA vaccines), doesn’t stop transmission or spread, has many deficiencies in the safety studies, is liability-free (no recourse for damages if you’re injured) vaccine, people really need to do a risk vs. reward analysis. If you are in a lower risk group, do you really want to take the risk, when the possible long-term effects with an entirely experimental vaccine will not be known for years? If you are at high risk for severe COVID-19 disease because you are very old, frail or have significant co-morbid metabolic disease, do you want to take the risk of the vaccine not knowing how your health condition will be affected by the vaccine? Or, would you rather assume the risk from COVID-19? That has to be a well thought out individual decision.
But back to the lockdown/quarantine discussion. By keeping everyone quarantined so stringently, we are only keeping our elderly isolated and away from their loved ones for a much, much longer period of time. But that strategy is also increasing their chances of infection, not only because they have so many more potential interactions with the virus over a 12 to 18-month period than in a normal respiratory viral infection cycle period, but because they are not seeing, hugging and being held by their loved ones. That prolonged isolation and lack of human touch is devastating to their immune system, not to mention the fear and loss of hope, all making them even more susceptible to harmful effects from the virus. Also consider, that according to the CDC, 50,000 to 80,000 people (over 80% of them elderly), die of the flu and pneumonia each year, they will also be at higher risk to those types of infections. In fact, the stark reality is that tens of thousands of those elderly casualties from COVID-19 would have passed away from other viral or bacterial upper respiratory infections in 2020 or early 2021 absent COVID-19. I’m not rationalizing that they would have died anyway, it’s just the honest but sad truth. The chart below shows in a very graphic way how susceptible the elderly are to death from all causes.
Another visual perspective
So, think about it in these terms. If you are 40 years old, had contracted COVID-19, picture yourself in a crowd of 5,000 people ALL WITH COVID-19. That’s a lot of people! As shown above, the statistics from the CDC indicate that only one of those 5,000 people would perish from COVID-19. If you’re looking over that sea of people, there would be only 1 that would die from it. What are the chances that 1 death would be you? It’s very unlikely that it is actually 1 in 5,000. It could be more, or it could be less. I’ll cover that in a minute.
If you are 18 years old and have COVID-19, you can picture yourself in a major league baseball stadium, packed with only children and teens ALL with COVID-19 infections like you. Statistically, only 1 of those 34,000 young people would die from COVID-19. And that child very likely would have had some underlying health condition that made them more susceptible to adverse effects from the disease.
How do those fatality statistics compare to a “normal” flu season? Influenza accounts for about 10% of all flu-and-pneumonia-combined deaths each year and pneumonia about 90% (the CDC now combines these 2 categories of deaths together in one category as Influenza & Pneumonia). The Case Fatality Rate (CFR) for the average flu season is 0.1%. That means that 1 in 1,000 people diagnosed with the flu/pneumonia will die from it. In a more lethal flu season 1 in 500 people may die from influenza or pneumonia. Compare that to the different age sorted categories above and you will see that statistically the flu is more dangerous to young and middle-aged people than the other seasonal respiratory infections that make up the Influenza & Pneumonia group. For COVID-19, approximately 81% of the deaths are in people age 65 and older, which is almost identical to the seasonal flu. https://www.cdc.gov/nchs/data/nvsr/nvsr65/nvsr65_04.pdf
According to an article written by Anthony Fauci, the Director of the National Institute of Allergy and Infectious Diseases (NIAID) and Robert Redfield the Head of the CDC published in the New England Journal of Medicine March 26, 2020, the fatality rate may be similar to a severe seasonal flu.
From the publication:
“If one assumes that the number of asymptomatic or minimally symptomatic cases is several times as high as the number of reported cases, the case fatality rate may be considerably less than 1%. This suggests that the overall clinical consequences of Covid-19 may ultimately be more akin to those of a severe seasonal influenza (which has a case fatality rate of approximately 0.1%) or a pandemic influenza (similar to those in 1957 and 1968) rather than a disease similar to SARS or MERS, which have had case fatality rates of 9 to 10% and 36%, respectively.” https://www.nejm.org/doi/full/10.1056/NEJMe2002387
My Note: The asymptomatic case estimates range between 40% and 60%. These people never see a doctor and are never diagnosed with COVID-19. Based on the studies I have seen, I believe that they are closer to the 60% number if T-Cell immunity and dormant B-cell levels from previous coronavirus specific common cold infections are taken into consideration. The lower range of 40% the CDC cites is based on antibody testing of general populations and don’t consider the T-cell and dormant B-cell immunity just mentioned (more details on this below). And importantly, the higher the percentage of asymptomatic “immune” people in the population, the lower the Infection Fatality Rate becomes because there are fewer “hosts” for the virus to infect.
More recently, an article titled CDC: COVID-19 Death Rate Far Lower Than Previously Thought, reports on the latest CDC projections. https://www.thenewamerican.com/usnews/health-care/item/35799-cdc-covid-19-death-rate-far-lower-than-previously-thought
From the article:
“The federal government is finally admitting what many observers have suspected all along: The average American’s chances of dying from COVID-19 are extremely small. The Centers for Disease Control and Prevention’s (CDC) latest best estimate of the death rate for individuals with COVID-19 symptoms is just 0.26 percent, slightly higher than that of the seasonal flu.” (That 0.26% number is for all age groups combined)
Risk of death grossly over-exaggerated
One of the world’s top epidemiologists from Stanford releases a new study showing that COVID-19 mortality reporting is greatly over-exaggerated
The author of a new peer-reviewed study is Dr. John P.A. Ioannidis, Professor of Medicine (Stanford Prevention Research), of Epidemiology and Population Health and by courtesy, of Statistics and of Biomedical Data Science. Department of Medicine – Stanford Prevention Research Center.
The study is titled, The infection fatality rate of COVID-19 inferred from seroprevalence data. It has recently been released in a bulletin from the World Health Organization and demonstrates that while the death rate from COVID-19 varies significantly in different countries, the death rate in people under 70 is much less than the seasonal flu and much lower than estimates earlier in the pandemic.
He included 61 studies (74 estimates) and eight preliminary national estimates and found that across 57 locations, the IFR was 0.23% and INCREDIBLY found that In people < 70 years, infection fatality rates ranged from 0.00% to 0.31% with crude and corrected medians of 0.05%!
https://www.medrxiv.org/content/10.1101/2020.05.13.20101253v3.full.pdf
Once again, facts not fear should inform your thoughts, opinions and decisions.
Lifestyle and co-morbidities as risk factors for death from COVID-19
A large study looking at 160 countries through August 31, 2020 and published November 19, 2020 in the journal Frontiers in Public Health titled, Covid-19 Mortality: A Matter of Vulnerability Among Nations Facing Limited Margins of Adaptation, tested major indices from five domains (demography, public health, economy, politics, environment) and their potential associations with Covid-19 mortality during the first 8 months of 2020. Some very interesting and insightful conclusions were made, including the first bullet point on lockdowns. Lockdowns have destroyed businesses, lives, families and economies, increased mental health problems, suicides, domestic and child abuse and deaths from despair, but it appears have not saved lives.
From the article:
https://www.frontiersin.org/articles/10.3389/fpubh.2020.604339/full
Each person must consider this crucial calculation-
Back to our 40-year-old. How healthy are you compared to the other 4,999 people?
This consideration will either give you a better than a 1 in 5,000 chance of survival, or a chance worse than that. The determining factor, is the degree you suffer from the following…
Sixty percent of adults suffer from at least one chronic disease. Forty percent have two or more.
This is undoubtably one of the key reasons why COVID-19 has hit countries like the U.S., that have high rates of chronic disease harder. The average person that has died from COVID-19 has 2.6 comorbidities per CDC..
These are the 4 most significant risk factors for severe outcome from COVID-19 and the percentage of American adults in that age group that have them: (Circle each one that you have been diagnosed with.)
- Hypertension- (45% of adults have it) https://www.cdc.gov/bloodpressure/facts.htm
(47.91 of fatal cases) https://pubmed.ncbi.nlm.nih.gov/32573311/
- Diabetes- (16% of adults have diabetes and 42% have pre-diabetes)
https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
(24.9% of fatal COVID-19 cases) https://pubmed.ncbi.nlm.nih.gov/32573311/
- Obesity- (42% of adults are obese) https://www.cdc.gov/nchs/data/databriefs/db360-h.pdf
(3X risk of hospitalization and increased risk of death) https://www.cdc.gov/obesity/data/obesity-and-covid-19.html (11.3% of fatal COVID-19 cases)
- Respiratory diseases-
(10.9% of fatal cases) https://pubmed.ncbi.nlm.nih.gov/32573311/
Numbers 5- 8 are also significant risk factors. Circle the ones that pertain to you.
- Kidney disease
- Smoking
- Being immunocompromised
- Non-Caucasian ethnicity– One established reason is that those with darker pigmented skin have lower levels of Vitamin D, which is a risk factor for severe COVID-19.
The following groups have increased risk of death from COVID-19 as compared to Caucasian and Asian Americans: African American (2.1X), Hispanic Americans (1.1X), Native Americans (1.4X). These ethnic groups also have higher rates of obesity, diabetes, cardiovascular disease than Caucasian and Asian Americans.
The risk of being hospitalized from COVID-19 is much higher for Black (4.7X), Hispanic (4.6X), Asian (1.3X) and Native Americans (5.3X) as compared to Caucasian Americans. https://www.cdc.gov/coronavirus/2019-ncov/downloads/covid-data/hospitalization-death-by-race-ethnicity.pdf
How many of those comorbidities and risk factors do you have?
The greater number of comorbidities, the greater your risk. The lower your number of comorbidities, the lower your risk. If you don’t have any of those comorbidities, your risk goes way down.
For more on the increased risks from various diseases and risk factors visit https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html#obesity
Back to the 40-year-old in the crowd of 5,000 infected with SARS-CoV-2. Since the prevalence of hypertension, diabetes and obesity are so high in the U.S., the numbers of people with one or more comorbidities in that crowd of 5,000 is probably greater than two-thirds of that crowd. Since their risk of experiencing a more severe case or death is so much greater than our healthy 40-year-old, it would essentially mean that the risk of death to the healthy person would be significantly less than the average risk the CDC stats specify. One may suppose that they may have around a 1 in 10,000 chance rather than a 1 in 5,000 chance of dying, because the odds of dying would be more likely in the unhealthiest of the unhealthy. This last example is not based on hard data but an estimate, simply to make the point that relatively healthy people, especially those under 70 years old have a much lower risk of death than the overall risk the CDC lists for their particular age group. And the younger the age demographic that we consider, the lower the risk becomes exponentially.
Risk of dying from COVID-19 compared to other risks we all assume daily
How does a 1 in 5,000 or 1 in 10,000 risk of COVID-19 compare with other risks we don’t even think about?
Lifetime odds of dying from:
- accidental drug poisoning- 1 in71
- opioids legal or illegal- 1 in 98
- a car accident- 1 in 106
- an assault by someone using a forearm- 1 in 298
- being hit by a car as a pedestrian- 1 in 541
- from exposure to smoke fire and flames- 1 in 1,399
- a fall down steps- 1 in 1,657
- Drowning after falling into a swimming pool- 1 in 5,573
The Insurance Information Institute– 2017 statistics
https://www.iii.org/fact-statistic/facts-statistics-mortality-risk
Now all of this is assuming that you contract COVID-19
Your risk of death drops even more when you consider that you may never contract COVID-19. Current research is demonstrating that a decent percentage of the population has some immunity to coronaviruses because of previous common cold infections people have had. Coronaviruses make up about 15-20 percent of infections that we call the common cold. Since SARS-CoV-2 is a “cousin” of the common cold coronaviruses and share many of the same protein antigens that our immune system recognizes, therefore signaling our immune system through T-cell and Innate immunity to seek and destroy the virus. T-cells, thwart infections in two different ways. Helper T cells stimulate B-cells and other immune defenders into action, whereas killer T-cells target and destroy infected cells. The severity of disease can depend on the strength of these T cell and overall Innate Immune responses. I have seen the growing body of scientific evidence regarding this phenomenon since the start of the pandemic. The bottom line is, even though SARS-CoV-2 in a “novel” (new) virus, it isn’t entirely novel and our immune systems have already met it’s cousins.
In a Science Magazine article published May 14, 2020 titled T cells found in COVID-19 patients ‘bode well’ for long-term immunity, researchers analyzed blood from 68 uninfected people and found that 34% hosted helper T cells that recognized SARS-CoV-2. The La Jolla team detected this cross-reactivity in about half of stored blood samples collected between 2015 and 2018, well before the current pandemic began. The researchers think these cells were likely triggered by past infection with one of the four human coronaviruses that cause colds; proteins in these viruses resemble those of SARS-CoV-2. The results suggest “one reason that a large chunk of the population may be able to deal with the virus is that we may have some small residual immunity from our exposure to common cold viruses,” says viral immunologist Steven Varga of the University of Iowa.
This is just one of numerous articles that have been published confirming this activity of “dormant” immune cells primed from other coronavirus infections that rise to the occasion against SARS-CoV-2. This is also another reason why many top scientists feel it will not be necessary for a majority of the population to be infected and develop antibodies or get a vaccine to boost antibodies before we reach herd immunity and the virus dwindles.
What level of population immunity will it require with SARS-CoV-2?
The R-Naught (R0 or Basic Reproduction Number) for an infectious disease event is the estimated number of people that an infected person will in turn infect. It is generally reported as a single numeric value or low–high range. An outbreak is expected to continue if R0 has a value >1 and to end if R0 is <1. It also is used to estimate the percentage of the population that would need to be “immune” from a disease to control its spread through the concept of herd or population immunity. The more infective the disease, the higher the percentage of the population would need to be immune. Measles for example is estimated to have an R0
somewhere between 12-18. Therefore, it is thought that the percentage of the population that would need to be immune to protect the rest would be around 90-95%. A virus with an R0 of 2-3 may only require 60% of the population to be immune to control the outbreak.
The R0 for the SARS-CoV-2 virus is estimated to be 2.5, as of the last published data from the CDC in August. As an infection works its way through the population that number will be expected to drop. The R0 for the seasonal flu ranges from 0.9-2.1. The common cold is estimated to be 2-3. Even with an infectibility rating near that of SARS-CoV-2, not everyone contracts the seasonal flu or the common cold each year. And, as larger numbers of the population become infected and recover, the number of susceptible hosts drop and the likelihood of getting infected drops. Eventually the virus “burns itself out”. That is what happened to SARS-CoV-1. A vaccine was never successfully developed and in fact the effort was abandoned because the trials never went beyond animal studies. The vaccine candidates caused severe adverse effects in the animal subjects and the efforts were dropped.
Even though cases were rising to all time highs in November, deaths were remaining relatively flat
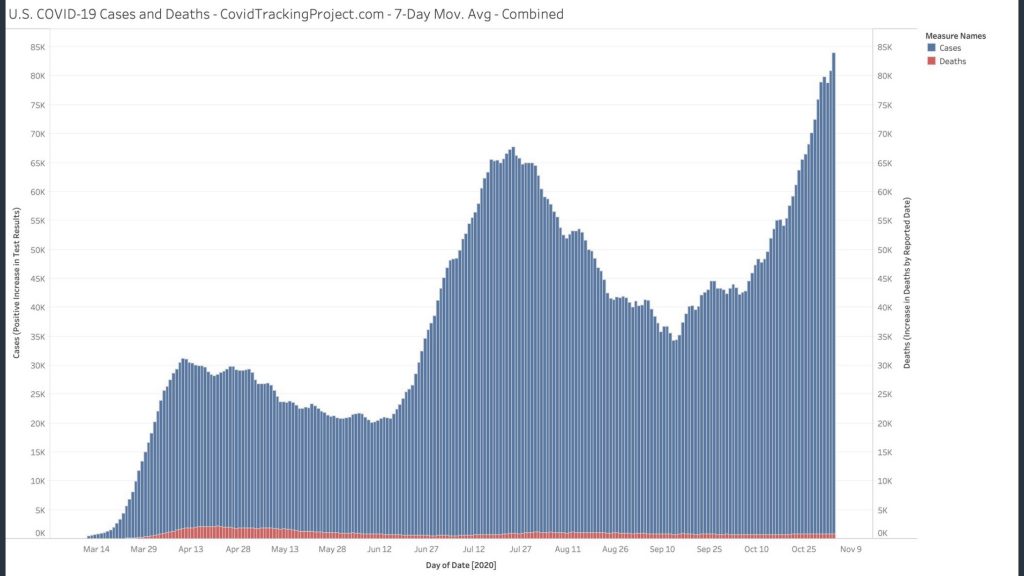
As can be seen clearly in the graphic, despite cases peaking (blue) at the highest rates since the pandemic deaths (red) are remaining relatively flat, especially in comparison to the northern states in late March to early May and the southern states mid-summer.
Think about the mainstream media and public health messaging as cases spike. Their message is, “cases are spiking, sound the alarm, hunker down, wear your masks and stay indoors”. Is it possible that as we march toward population/community/herd immunity, we are seeing the mortality rates flatten? This is very good news indeed!
Cases and hospital capacity
A November 3rd Tweet by Dr. Scott Atlas, one of the President’s Coronavirus Task Force members gave additional encouragement when he said the following:
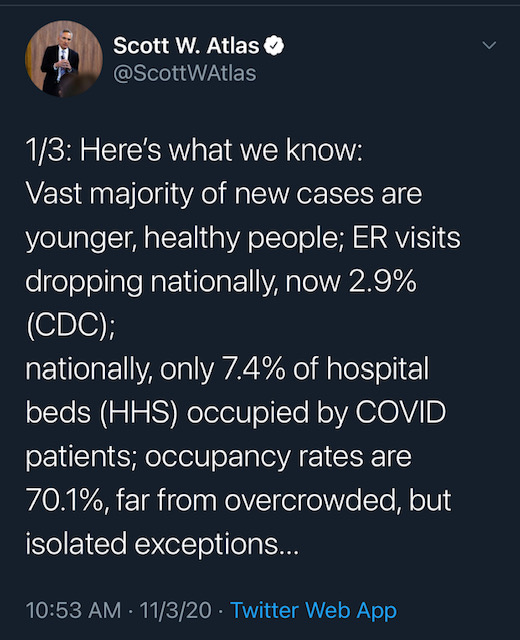
He went on to say that they hospitals are now well supplied with PPE, better infection control, better protection of seniors, mortality rate down 85% since April…. These are all great developments that should also alleviate excess fear.
The bottom line on risk
Yes, life IS RISKY. But we go on with life accepting risk every day. Should we live in a bubble, or in our basements never to emerge? To hide from all risk, is to stop living.
Aside from that, studies and data from around the world are showing that the death rates of hospitalized patients are going down significantly. Remember, the survivability statistics above were from the beginning of August. In the last 4 months, survivability has improved even more. Doctors are figuring out the best treatment options based on what we now know. That is making a real difference. And early intervention with Hydroxychloroquine and zinc, Ivermectin, inhaled steroids at the appropriate time, or in lower risk patients Quercetin or EGCG and zinc, is reducing the number of people that need to be hospitalized. And, of course maintaining optimal Vitamin D levels is an incredibly important preventative measure. You can see excerpts and references from several dozen studies showing the power of Vitamin D levels in preventing and lowering severity of viral respiratory infections including COVID-19 at my website HERE. (https://www.wellnessdoc.com/vitamin-d-status-as-it-relates-to-covid-19-complications-and-death/ )
Each person must decide what their risk tolerance is, but everyone should look at their particular risk based on all I have mentioned. Don’t let the mainstream media, the health agencies whose job is to make you afraid of any risk and the political factions who have a vested interest in keeping you afraid, succeed. Be rational. Look at the true risks FOR YOU as an individual based on the evidence. Act accordingly. Be smart and don’t let unreasonable fear keep you from enjoying life.
Being proactive with your health is a strong defense
The one thing I can say unequivocally, is that for individuals who have invested their life in pursuing a healthy lifestyle, healthy diet, nutritional supplements and exercise, all of those disciplines are paying HUGE dividends right now. For those of you that are interested in finding out how I may be able to help you change your risk profile through all of those things I just mentioned, contact me through my web site at https://wellnessdoc.com and follow the Expert Advice tab to 1-on1 Coaching. I would love to help you set up a strategic game plan to help you accomplish that.
Check out Dr. Palmer’s downloadable eBook 1200 Studies- Truth will Prevail. It is now at 737 pages, with excerpts and summaries from over 1,400 published studies authored by thousands of scientists and researchers, that contradict what the public is being told about the safety and efficacy of vaccines. It has easy search and navigation features with links directly to the article abstracts on PubMed, or the source journal. These features make it an invaluable research and reference tool. It can be downloaded at https://1200studies.com
Other references mentioned in the article:
- Asymptomatic people do not spread the virus- A study involving nearly 10 million people
Post-lockdown SARS-CoV-2 nucleic acid screening in nearly ten million residents of Wuhan, China
https://pubmed.ncbi.nlm.nih.gov/33219229/
- Face masks do not stop spread to a statistically significant level
Effectiveness of Adding a Mask Recommendation to Other Public Health Measures to Prevent SARS-CoV-2 Infection in Danish Mask Wearers
https://www.acpjournals.org/doi/10.7326/M20-6817
- Lockdowns do not reduce mortality– A study involving 160 countries
Covid-19 Mortality: A Matter of Vulnerability Among Nations Facing Limited Margins of Adaptation
https://www.frontiersin.org/articles/10.3389/fpubh.2020.604339/full